Health systems are seeing changing demands on their existing ambulatory asset portfolio, in both services offered and facilities needed. As systems move to meet patients where they are in their health journey and see a continued shifting of services to the ambulatory settings, there are four key aspects to consider in refining and redefining one’s ambulatory portfolio.
1. Future Strategic Goals
A health system’s assets include not only its physical assets but also its service lines, and it is critical to understand the market’s need from a service perspective. A key layer in asset planning is developing a strategy around service line growth or reduction based on market demand and market capture. This strategy helps substantiate investment in providers to serve a community with a specific stratification of service needs and can show where a service may already be saturated with providers beyond what the market needs. A competitor analysis can also assist in understanding where and how additional investment in providers can shift market share in a health system’s favor or where a service line may not be appropriate for additional investment. Service location analysis can provide an additional layer of consideration when asset planning, enabling administrative teams to strategically locate assets within communities to strengthen networks, meet consumers where they are, and create easy access points to the health system.

Primary care is a good example of a service that acts as a front door to a health system. While it may be less lucrative than specialty services, it provides a necessary community service and is ideally located within the community rather than adjacent to the hospital campus. Analyzing the market dynamics around primary care services and providing the right assets for the community can lead to consumer support throughout their health journey while managing your market’s healthcare consumption.
2. Operational Targets and Organizational Culture
Integrating providers’ operational expectations into an analysis of asset needs is paramount in determining physical space needs to support a market. Some health systems have specific productivity metrics for providers to meet, while others may not. An analysis of the current conditions can highlight providers’ available capacity or constraints. When calculating space needs, it’s important to build in intended operational parameters with flexibility, knowing that care models will adjust in the future as consumers’ needs change. The demands of telehealth on providers’ available time can affect the capacity for in-person visits and should be accounted for in the evaluation. Patient procession and staff workflows are integral in an efficient operational model and space utilization. Efficient operations lead to an efficient utilization of square footage and can often require fewer exam rooms than originally conceived.

Overlaying operational expectations for providers and market demands can provide additional clarity around network distribution. An asset review may be an opportune time for organizations to shift providers around their region to better serve their consumers.
An organization’s culture around space utilization can have a dramatic impact on future space needs. Practice culture can dictate whether providers have dedicated exam and support space or if they are sharing between providers or even between practices. In a shared environment, organizations can maximize the utilization of each exam room versus dedicating rooms to providers who may not be in the clinic every day or hour it is open to see patients. Taking providers and staff members along the journey to rethinking their space can help them understand the inherent savings created when spaces are shared. This can also create innovation in finding alternative ways to use space when a provider is not in clinic while still providing them the operations of dedicated rooms while in clinic.
3. Conditions of Existing Assets
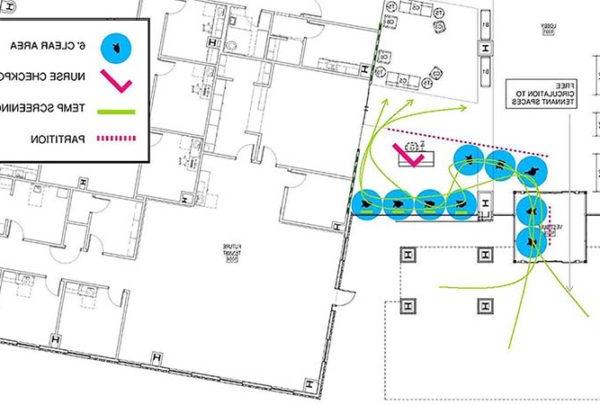
In any asset study, it is key to have a grasp of the conditions of the existing facilities that are part of the study to help clarify the conditions the practices are working in today. Assessing the conditions of facilities should be conducted in a methodical manner to be able to compare the buildings’ viability for future use. Both architectural and engineering assessments should be completed; a building may appear at the surface acceptable, but on further investigation the infrastructure may not be able to support future needs or may require financial investment beyond what the organization is willing to accommodate. Assessments can be conducted at a variety of depths of investigation; the key is to be consistent across all assets for an even comparison.

Part of assessing a facility is comparing it to industry standards and current codes for compliance and space allotment. This will help the team understand how the practice/department is currently utilizing the square footage available to them. This evaluation can also highlight deficiencies or excesses in certain areas of the program that may be creating operational challenges for the users. Buildings may not be required to be brought up to current codes for continued use as is; however, understanding where deficiencies are will help the owner understand where future financial investment may be required.
Creating a matrix of findings enables a quick view of how facility assets stack up against each other and against what the future use of that building may be. This also helps quickly visualize which buildings are worth salvaging versus divesting.
4. Financial Investment
Assessment of the financial viability of changes to ambulatory assets underpins the organization’s ability to enhance and align their service offerings. Most facilities will require continued investment for maintenance, enhancements, and general wear and tear that occur over the life of a building. However, additional investments may be needed to relocate, expand, or right-size service lines. Financial viability ultimately determines how a health system moves forward with any plans. Investment in a service line must balance how much is invested with how much revenue will be realized. If those factors don’t balance, the investment may not be worth the outcome. Investing in a new building or a big renovation needs to generate enough revenue to help cover the cost of that project over time.

Ambulatory asset planning is a puzzle with multiple moving parts that will determine whether it’s worthwhile to make a financial investment in a service line or building. Finding the best alignment with a practice’s needs and what the facilities have to offer will ultimately determine the success of the ambulatory asset plan.